Cancer vaccines are having a renaissance
This article first appeared in The Checkup, MIT Technology Review’s weekly biotech newsletter. To receive it in your inbox every Thursday, and read articles like this first, sign up here.
Last week, Moderna and Merck launched a large clinical trial in the UK of a promising new cancer therapy: a personalized vaccine that targets a specific set of mutations found in each individual’s tumor. This study is enrolling patients with melanoma. But the companies have also launched a phase III trial for lung cancer. And earlier this month BioNTech and Genentech announced that a personalized vaccine they developed in collaboration shows promise in pancreatic cancer, which has a notoriously poor survival rate.
Drug developers have been working for decades on vaccines to help the body’s immune system fight cancer, without much success. But promising results in the past year suggest that the strategy may be reaching a turning point. Will these therapies finally live up to their promise?
This week in The Checkup, let’s talk cancer vaccines. (And, you guessed it, mRNA.)
Long before companies leveraged mRNA to fight covid, they were developing mRNA vaccines to combat cancer. BioNTech delivered its first mRNA vaccines to people with treatment-resistant melanoma nearly a decade ago. But when the pandemic hit, development of mRNA vaccines jumped into warp drive. Now dozens of trials are underway to test whether these shots can transform cancer the way they did covid.
Recent news has some experts cautiously optimistic. In December, Merck and Moderna announced results from an earlier trial that included 150 people with melanoma who had undergone surgery to have their cancer removed. Doctors administered nine doses of the vaccine over about six months, as well as what’s known as an immune checkpoint inhibitor. After three years of follow-up, the combination had cut the risk of recurrence or death by almost half compared with the checkpoint inhibitor alone.
The new results reported by BioNTech and Genentech, from a small trial of 16 patients with pancreatic cancer, are equally exciting. After surgery to remove the cancer, the participants received immunotherapy, followed by the cancer vaccine and a standard chemotherapy regimen. Half of them responded to the vaccine, and three years after treatment, six of those people still had not had a recurrence of their cancer. The other two had relapsed. Of the eight participants who did not respond to the vaccine, seven had relapsed. Some of these patients might not have responded because they lacked a spleen, which plays an important role in the immune system. The organ was removed as part of their cancer treatment.
The hope is that the strategy will work in many different kinds of cancer. In addition to pancreatic cancer, BioNTech’s personalized vaccine is being tested in colorectal cancer, melanoma, and metastatic cancers.
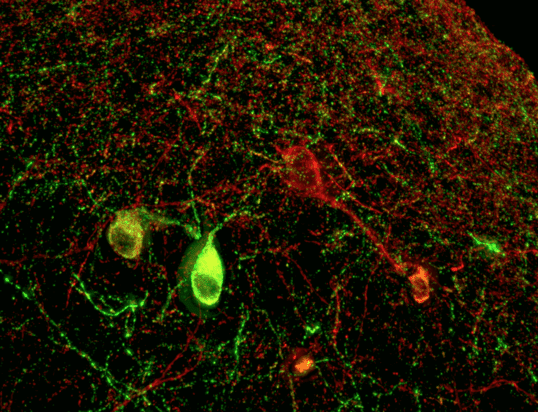
The purpose of a cancer vaccine is to train the immune system to better recognize malignant cells, so it can destroy them. The immune system has the capacity to clear cancer cells if it can find them. But tumors are slippery. They can hide in plain sight and employ all sorts of tricks to evade our immune defenses. And cancer cells often look like the body’s own cells because, well, they are the body’s own cells.
There are differences between cancer cells and healthy cells, however. Cancer cells acquire mutations that help them grow and survive, and some of those mutations give rise to proteins that stud the surface of the cell—so-called neoantigens.
Personalized cancer vaccines like the ones Moderna and BioNTech are developing are tailored to each patient’s particular cancer. The researchers collect a piece of the patient’s tumor and a sample of healthy cells. They sequence these two samples and compare them in order to identify mutations that are specific to the tumor. Those mutations are then fed into an AI algorithm that selects those most likely to elicit an immune response. Together these neoantigens form a kind of police sketch of the tumor, a rough picture that helps the immune system recognize cancerous cells.
“A lot of immunotherapies stimulate the immune response in a nonspecific way—that is, not directly against the cancer,” said Patrick Ott, director of the Center for Personal Cancer Vaccines at the Dana-Farber Cancer Institute, in a 2022 interview. “Personalized cancer vaccines can direct the immune response to exactly where it needs to be.”
How many neoantigens do you need to create that sketch? “We don’t really know what the magical number is,” says Michelle Brown, vice president of individualized neoantigen therapy at Moderna. Moderna’s vaccine has 34. “It comes down to what we could fit on the mRNA strand, and it gives us multiple shots to ensure that the immune system is stimulated in the right way,” she says. BioNTech is using 20.
The neoantigens are put on an mRNA strand and injected into the patient. From there, they are taken up by cells and translated into proteins, and those proteins are expressed on the cell’s surface, raising an immune response
mRNA isn’t the only way to teach the immune system to recognize neoantigens. Researchers are also delivering neoantigens as DNA, as peptides, or via immune cells or viral vectors. And many companies are working on “off the shelf” cancer vaccines that aren’t personalized, which would save time and expense. Out of about 400 ongoing clinical trials assessing cancer vaccines last fall, roughly 50 included personalized vaccines.
There’s no guarantee any of these strategies will pan out. Even if they do, success in one type of cancer doesn’t automatically mean success against all. Plenty of cancer therapies have shown enormous promise initially, only to fail when they’re moved into large clinical trials.
But the burst of renewed interest and activity around cancer vaccines is encouraging. And personalized vaccines might have a shot at succeeding where others have failed. The strategy makes sense for “a lot of different tumor types and a lot of different settings,” Brown says. “With this technology, we really have a lot of aspirations.”
Now read the rest of The Checkup
Read more from MIT Technology Review’s archive
mRNA vaccines transformed the pandemic. But they can do so much more. In this feature from 2023, Jessica Hamzelou covered the myriad other uses of these shots, including fighting cancer.
This article from 2020 covers some of the background on BioNTech’s efforts to develop personalized cancer vaccines. Adam Piore had the story.
Years before the pandemic, Emily Mullin wrote about early efforts to develop personalized cancer vaccines—the promise and the pitfalls.
From around the web
Yes, there’s bird flu in the nation’s milk supply. About one in five samples had evidence of the H5N1 virus. But new testing by the FDA suggests that the virus is unable to replicate. Pasteurization works! (NYT)
Studies in which volunteers are deliberately infected with covid—so-called challenge trials—have been floated as a way to test drugs and vaccines, and even to learn more about the virus. But it turns out it’s tougher to infect people than you might think. (Nature)
When should women get their first mammogram to screen for breast cancer? It’s a matter of hot debate. In 2009, an expert panel raised the age from 40 to 50. This week they lowered it to 40 again in response to rising cancer rates among younger women. Women with an average risk of breast cancer should get screened every two years, the panel says. (NYT)
Wastewater surveillance helped us track covid. Why not H5N1? A team of researchers from New York argues it might be our best tool for monitoring the spread of this virus. (Stat)
Long read: This story looks at how AI could help us better understand how babies learn language, and focuses on the lab I covered in this story about an AI model trained on the sights and sounds experienced by a single baby. (NYT)