My biotech plants are dead
This article first appeared in The Checkup, MIT Technology Review’s weekly biotech newsletter. To receive it in your inbox every Thursday, and read articles like this first, sign up here.
Six weeks ago, I pre-ordered the “Firefly Petunia,” a houseplant engineered with genes from bioluminescent fungi so that it glows in the dark.
After years of writing about anti-GMO sentiment in the US and elsewhere, I felt it was time to have some fun with biotech. These plants are among the first direct-to-consumer GM organisms you can buy, and they certainly seem like the coolest.
But when I unboxed my two petunias this week, they were in bad shape, with rotted leaves. And in a day, they were dead crisps. My first attempt to do biotech at home is a total bust, and it cost me $84, shipping included.
My plants did arrive in a handsome black box with neon lettering that alerted me to the living creature within. The petunias, about five inches tall, were each encased in a see-through plastic pod to keep them upright. Government warnings on the back of the box assured me they were free of Japanese beetles, sweet potato weevils, the snail Helix aspera, and gypsy moths.
The problem was when I opened the box. As it turns out, I left for a week’s vacation in Florida the same day that Light Bio, the startup selling the petunia, sent me an email saying “Glowing plants headed your way,” with a UPS tracking number. I didn’t see the email, and even if I had, I wasn’t there to receive them.
That meant my petunias sat in darkness for seven days. The box became their final sarcophagus.
My fault? Perhaps. But I had no idea when Light Bio would ship my order. And others have had similar experiences. Mat Honan, the editor in chief of MIT Technology Review, told me his petunia arrived the day his family flew to Japan. Luckily, a house sitter feeding his lizard eventually opened the box, and Mat reports the plant is still clinging to life in his yard.

But what about the glow? How strong is it?
Mat says so far, he doesn’t notice any light coming from the plant, even after carrying it into a pitch-dark bathroom. But buyers may have to wait a bit to see anything. It’s the flowers that glow most brightly, and you may need to tend your petunia for a couple of weeks before you get blooms and see the mysterious effect.
“I had two flowers when I opened mine, but sadly they dropped and I haven’t got to see the brightness yet. Hoping they will bloom again soon,” says Kelsey Wood, a postdoctoral researcher at the University of California, Davis.
She would like to use the plants in classes she teaches at the university. “It’s been a dream of synthetic biologists for so many years to make a bioluminescent plant,” she says. “But they couldn’t get it bright enough to see with the naked eye.”
Others are having success right out of the box. That’s the case with Tharin White, publisher of EYNTK.info, a website about theme parks. “It had a lot of protection around it and a booklet to explain what you needed to do to help it,” says White. “The glow is strong, if you are [in] total darkness. Just being in a dark room, you can’t really see it. That being said, I didn’t expect a crazy glow, so [it] meets my expectations.”
That’s no small recommendation coming from White, who has been a “cast member” at Disney parks and an operator of the park’s Avatar ride, named after the movie whose action takes place on a planet where the flora glows. “I feel we are leaps closer to Pandora—The World of Avatar being reality,” White posted to his X account.
Chronobiologist Brian Hodge also found success by resettling his petunia immediately into a larger eight-inch pot, giving it flower food and a good soaking, and putting it in the sunlight. “After a week or so it really started growing fast, and the buds started to show up around day 10. Their glow is about what I expected. It is nothing like a neon light but more of a soft gentle glow,” says Hodge, a staff scientist at the University of California, San Francisco.
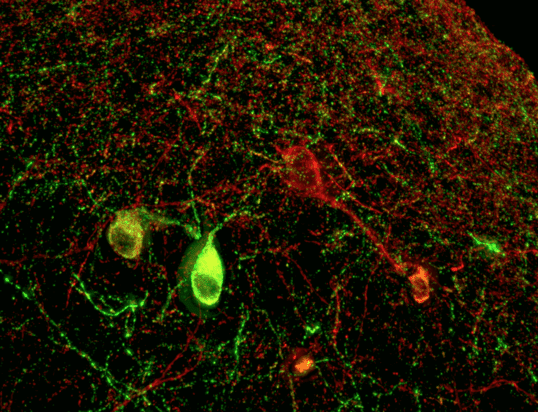
In his daily work, Hodge has handled bioluminescent beings before—bacteria mostly—and says he always needed photomultiplier tubes to see anything. “My experience with bioluminescent cells is that the light they would produce was pretty hard to see with the naked eye,” he says. “So I was happy with the amount of light I was seeing from the plants. You really need to turn off all the lights for them to really pop out at you.”
Hodge posted a nifty snapshot of his petunia, but only after setting his iPhone for a two-second exposure.
Light Bio’s CEO Keith Wood didn’t respond to an email about how my plants died, but in an interview last month he told me sales of the biotech plant had been “viral” and that the company would probably run out of its initial supply. To generate new ones, it hires commercial greenhouses to place clippings in water, where they’ll sprout new roots after a couple of weeks. According to Wood, the plant is “a rare example where the benefits of GM technology are easily recognized and experienced by the public.”
Hodge says he got interested in the plants after reading an article about combating light pollution by using bioluminescent flora instead of streetlamps. As a biologist who studies how day and night affect life, he’s worried that city lights and computer screens are messing with natural cycles.
“I just couldn’t pass up being one of the first to own one,” says Hodge. “Once you flip the lights off, the glow is really beautiful … and it sorta feels like you are witnessing something out of a futuristic sci-fi movie!”
It makes me tempted to try again.
Now read the rest of The Checkup
From the archives
We’re not sure if rows of glowing plants can ever replace streetlights, but there’s no doubt light pollution is growing. Artificial light emissions on Earth grew by about 50% between 1992 and 2017—and as much as 400% in some regions. That’s according to Shel Evergreen,in his story on the switch to bright LED streetlights.
It’s taken a while for scientists to figure out how to make plants glow brightly enough to interest consumers. In 2016, I looked at a failed Kickstarter that promised glow-in-the-dark roses but couldn’t deliver.
Another thing
Cassandra Willyard is updating us on the case of Lisa Pisano, a 54-year-old woman who is feeling “fantastic” two weeks after surgeons gave her a kidney from a genetically modified pig. It’s the latest in a series of extraordinary animal-to-human organ transplants—a technology, known as xenotransplantation, that may end the organ shortage.
From around the web
Taiwan’s government is considering steps to ease restrictions on the use of IVF. The country has an ultra-low birth rate, but it bans surrogacy, limiting options for male couples. One Taiwanese pair spent $160,000 to have a child in the United States. (CNN)
Communities in Appalachia are starting to get settlement payments from synthetic-opioid makers like Johnson & Johnson, which along with other drug vendors will pay out $50 billion over several years. But the money, spread over thousands of jurisdictions, is “a feeble match for the scale of the problem.” (Wall Street Journal)
A startup called Climax Foods claims it has used artificial intelligence to formulate vegan cheese that tastes “smooth, rich, and velvety,” according to writer Andrew Rosenblum. He relates the results of his taste test in the new “Build” issue of MIT Technology Review. But one expert Rosenblum spoke to warns that computer-generated cheese is “significantly” overhyped.
AI hype continued this week in medicine when a startup claimed it has used “generative AI” to quickly discover new versions of CRISPR, the powerful gene-editing tool. But new gene-editing tricks won’t conquer the main obstacle, which is how to deliver these molecules where they’re needed in the bodies of patients. (New York Times).