This company plans to transplant gene-edited pig hearts into babies next year
The baby baboon is wearing a mesh gown and appears to be sitting upright. “This little lady … looks pretty philosophical, I would say,” says Eli Katz, who is showing me the image over a Zoom call.
This baboon is the first to receive a heart transplant from a young gene-edited pig as part of a study that should pave the way for similar transplants in human babies, says Katz, chief medical officer at the biotech company eGenesis.
The company, based in Cambridge, Massachusetts, has developed a technique that uses the gene-editing tool CRISPR to make around 70 edits to a pig’s genome. These edits should allow the organs to be successfully transplanted into people, the team says. As soon as next year, eGenesis hopes to transplant pig hearts into babies with serious heart defects. The goal is to buy them more time to wait for a human heart.
Before that happens, the team at eGenesis will practice on 12 infant baboons. Two such surgeries have been performed so far. Neither animal survived beyond a matter of days.
But the company is optimistic, as are others in the field. Many recipients of the first liver transplants didn’t survive either—but thousands of people have since benefited from such transplants, says Robert Montgomery, director of the NYU Langone Transplant Institute, who has worked with rival company United Therapeutics. Babies born with heart conditions represent “a great population to be focusing on,” he says, “because so many of them die.”
Editing risk
Over 100,000 people in the US alone are waiting for an organ transplant. Every day, around 17 of them die. Researchers are exploring multiple options, including the possibility of bioprinting organs or growing new ones inside people’s bodies. Transplanting animal organs is another potential alternative to help meet the need.
The idea of using organs and tissues from animals, known as xenotransplantation, is an old one—the first experiments were performed back in the 17th century. More recent attempts were made in the 1960s, and again in the 1990s. Many of these used organs from monkeys and baboons. But toward the start of the 1990s, a consensus emerged that pigs were the best donor candidates, says Montgomery.
Primates are precious—they are intelligent animals that experience complex emotions. Only a small number can be used for human research, and at any rate, they reproduce slowly. They are also more likely to be able to pass on harmful viruses. On the other hand, people already know a lot about how to rear and farm pigs, and their organs are about the right size for humans.
But transferring organs between animals of different species isn’t straightforward. Even organs from another human can be rejected by a recipient’s immune system, and animal tissues have a lot more components that our immune systems will regard as “foreign.” This can cause the organ to be attacked by immune cells. There’s also the possibility of transferring a virus along with the organ, for example. Even if a donor animal isn’t infected, it will have “endogenous retroviruses”—genetic code for ancient viruses that have long since been incorporated into its DNA.
These viruses don’t cause problems for their animal hosts. But there’s a chance they could cause an infection in another species. “There’s a risk that viruses that are endemic to animals evolve in a human and become deadly,” says Chris Gyngell, a bioethicist at Murdoch Children’s Research Institute in Melbourne, Australia.
The team at eGenesis is using CRISPR to address this risk. “You can use CRISPR-Cas9 to inactivate the 50 to 70 copies of retrovirus in the genome,” says Mike Curtis, president and chief executive officer at eGenesis. The edits prevent retroviruses from being able to replicate, he says.
Scientists at the company perform other gene edits, too. Several serve to “knock out” pig genes whose protein products trigger harmful immune responses in humans. And the team members insert seven human genes, which they believe should reduce the likelihood that the organ will be rejected by a human recipient’s immune system. In all, “we’re producing [organ] donors with over 70 edits,” says Curtis.
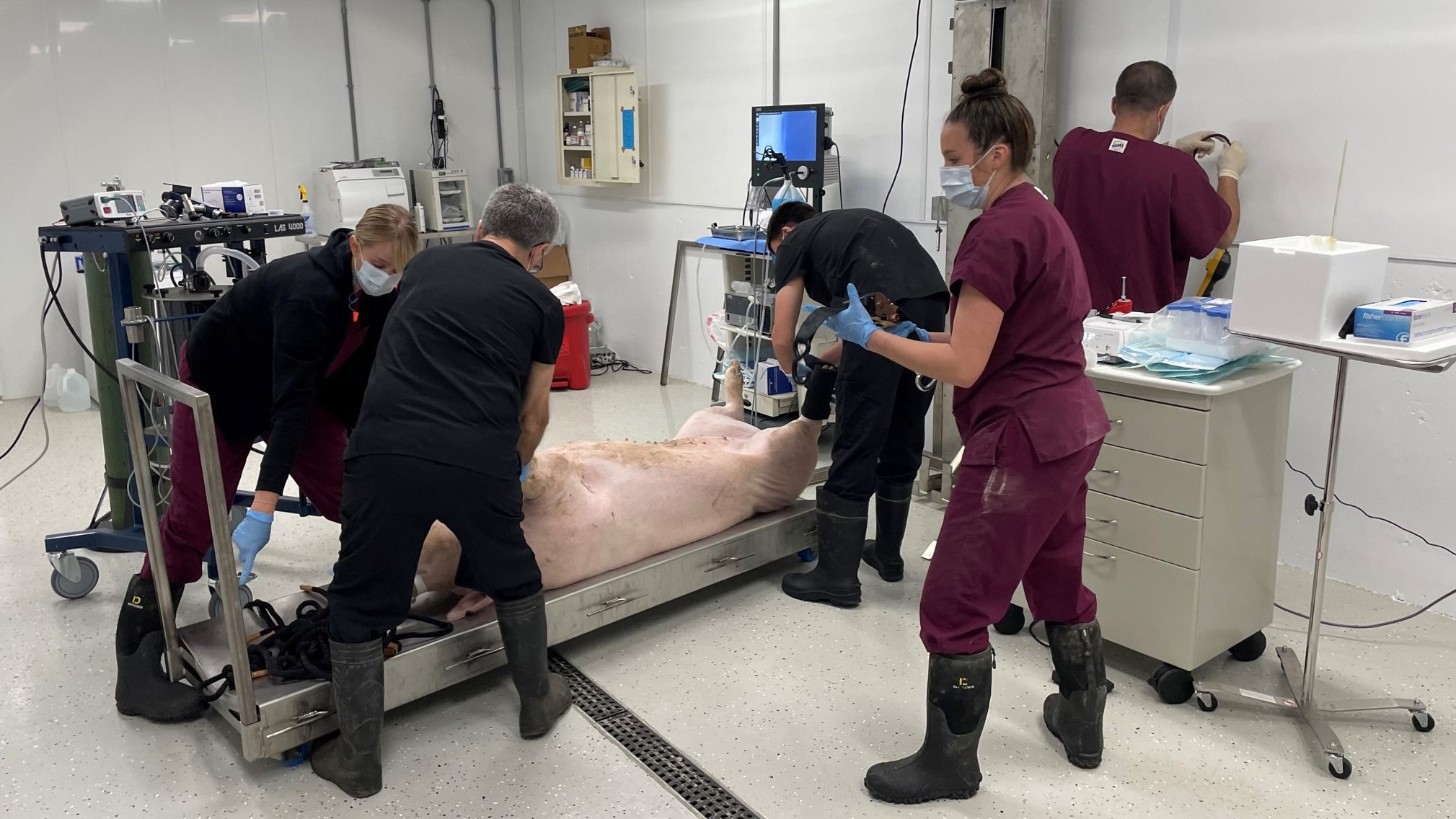
The team performs these edits on pig fibroblasts—cells that are found in connective tissue. Then they take the DNA-containing nuclei of edited cells and put them into pig egg cells. Once an egg is fertilized with sperm, the resulting embryo is implanted into the uterus of an adult pig. Eventually, cloned piglets are delivered by C-section. “It’s the same technology that was used to clone Dolly back in the ’90s,” says Curtis, referring to the famous sheep that was the first animal cloned from an adult cell.
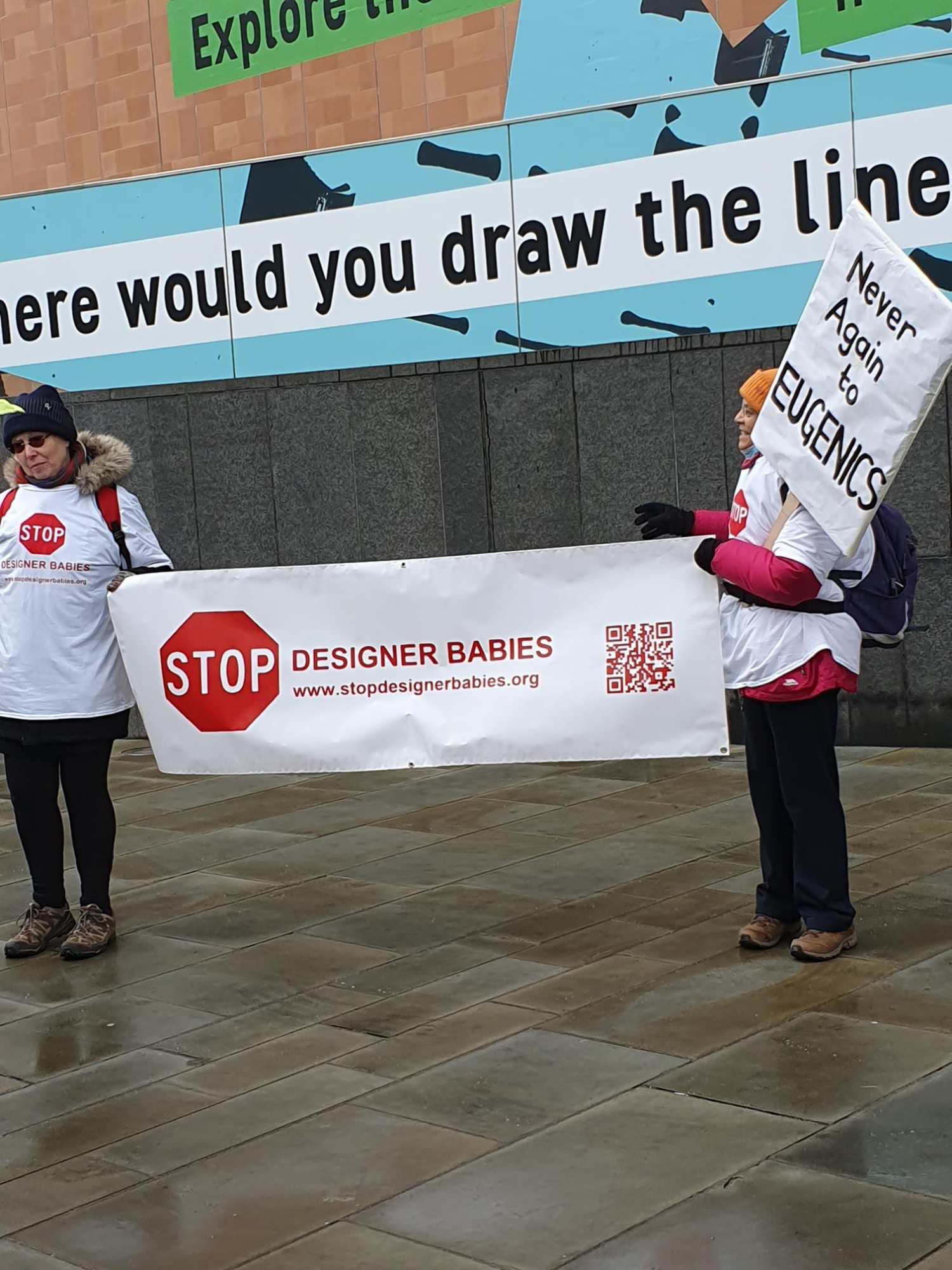
eGenesis has around 400 cloned pigs housed at a research facility in the Midwest (he is reluctant to reveal the exact location because facilities have been targeted by animal rights protesters). And early last year, the company set up a “clean” facility to produce organs fit for humans. Anyone who enters has to shower and don protective gear to avoid bringing in any bugs that might infect the pigs. The 200 pigs currently at this center live in groups of 15 to 25, says Curtis: “It’s basically like a very clean barn. We control all the feed that comes in, and we have waste control and airflow control.” There’s no mud.
The pigs that don’t end up having their organs used will be closely studied, says Curtis. The company needs to understand how the numerous gene edits they implement affect an animal over the course of its life. The team also wants to know if the human genes continue to be expressed over time. Some of the pigs are over four years old, says Curtis. “So far, it looks good,” he adds.
Complications
When it comes to organ transplants, size is important. Surgeons take care to match the size of a donor’s heart to that of the recipient. Baby baboons are small—only hearts taken from pigs aged one to two months old are suitable, says Curtis. Once they are transplanted, the hearts are expected to grow with the baboons.
The first baboon to get a pig heart, which was just under a year old, died within a day of surgery. “It was a surgical complication,” says Curtis. The intravenous tube providing essential fluids to the baboon became blocked, he says. “The animal had to be euthanized.”
A second baboon was operated on a few months later. The team encountered another surgical complication: this time, the surgeons couldn’t get the baboon’s blood vessels to stay attached to those in the pig’s organs. The baboon died nine days after the operation.
In both cases, “the heart itself was beating well,” says Curtis. “So far, the first two are very encouraging from cardiac performance … the hearts look good.” The surgeons who performed the operations are confident they’ll be able to avoid the surgical complications in the future, he says.
Tough decisions
Once the baboon trial is completed, the team at eGenesis wants to offer the pig hearts to babies under the age of two who were born with severe heart conditions. Such children have limited treatment options—human hearts of the right size are few and far between, and some of the devices used to treat heart conditions in adults aren’t suitable for little children with small hearts.
Curtis hopes the pig hearts could initially be used as a temporary measure for such children—essentially buying them more time to wait for a donated human heart. Once a potential recipient has been found, the company can seek approval for the surgery from the US Food and Drug Administration.
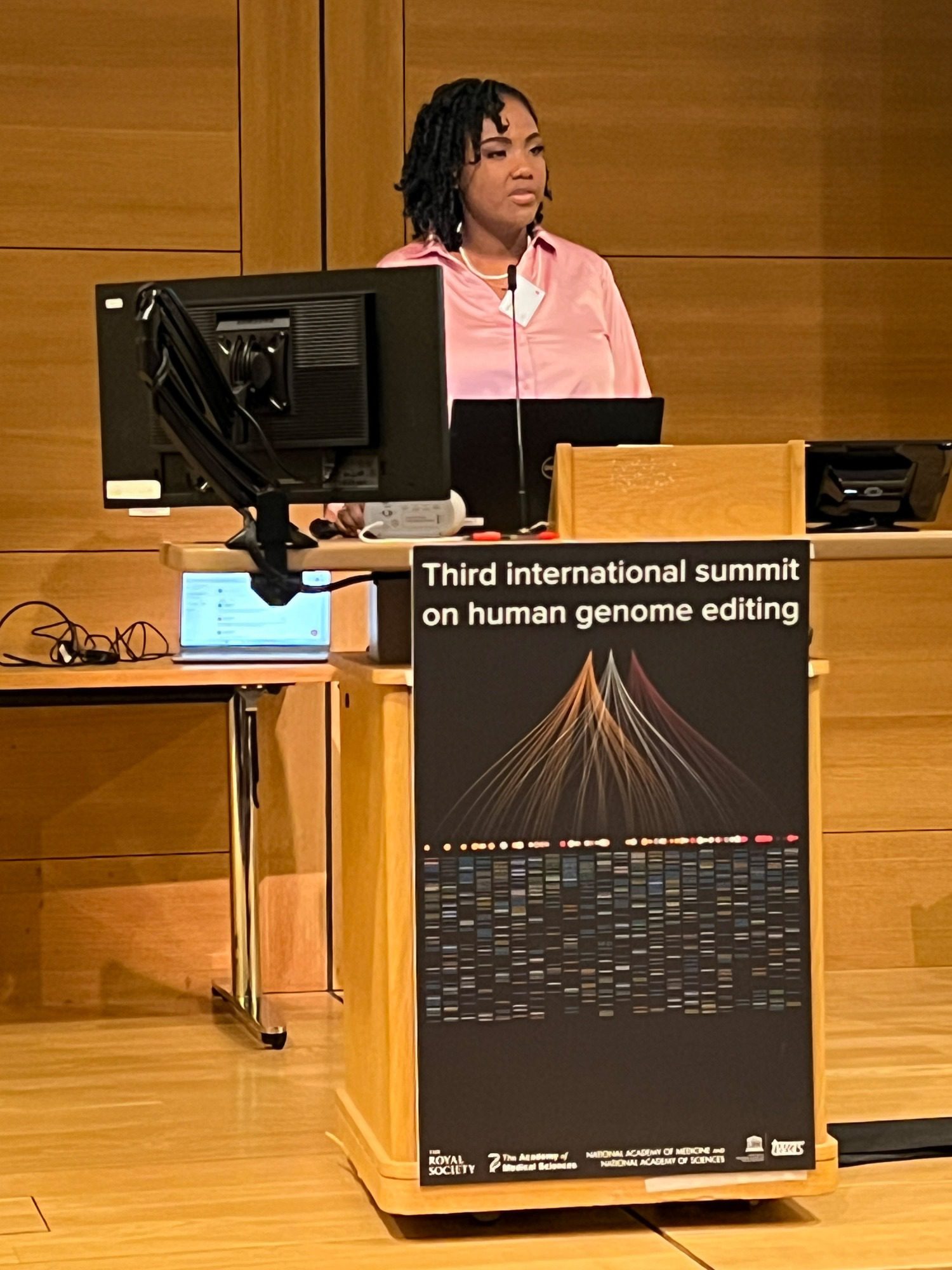
Ethicists will point out that babies won’t be able to give informed consent for surgery. That decision will come down to their caregiver, who will likely be in a dire situation, says Syd Johnson, a bioethicist at Upstate Medical University in Syracuse, New York. “These are parents who are desperate for anything that might save their child’s life,” she says.
But Gyngell thinks the focus should be on who has the most to gain from an experimental procedure like this. “The fact is that pediatric patients have a greater clinical need, because there are far fewer other options available to them,” he says.
Montgomery, who is himself the recipient of a donated human heart, agrees. He says he supports eGenesis’s goals. “These babies that have congenital heart disease … have a 50% mortality rate,” he says. “It’s a flip of a coin whether that kid is going to live or not.”
That reasoning doesn’t wash with Johnson. The procedure is risky, and a child whose immune system rejects the organ could suffer, she says: “One hundred percent of the patients who’ve been transplanted with an animal organ have died [soon after the procedure]—that’s just an inescapable fact.” David Bennett Sr., who was the first living person to receive a gene-edited pig heart, in 2022, died two months later.
There are more risks when using organs from gene-edited animals, says Johnson. We still don’t know if these genetic modifications might affect human recipients, especially in the long term. “The desire to do something to save these babies [with heart conditions] is obviously very strong for everyone who is involved,” she says. “But we still need to be honest and transparent about what the risks are—and they are, to some extent, unknown.”
Montgomery himself has transplanted gene-edited pig organs into adults who have been declared brain dead. Those organs—which include kidneys and, in unpublished work, hearts—were from pigs bred by the rival company Revivicor, which was acquired by United Therapeutics. The experiments ran for just two or three days, but Montgomery plans to run a similar experiment in individuals who will be studied for a month after the transplant. So far, he says, “we’ve got very good results.”
He believes young children may be better candidates for pig organs than adults, because their immune systems are still developing and therefore might be less likely to reject the organ. “They may well have some level of tolerance,” he says.
A third baboon is due to receive a pig heart in August. The company plans to perform at least one such operation a month until 12 animals have been operated on. The team members hope they’ll be able to fix the surgical issues and enable the baboons to live longer. Some other non-human primates that have received kidneys from the gene-edited pigs have already survived over a year, says Curtis.
“When you’re pioneering something new, there’s a steep learning curve,” Montgomery says.